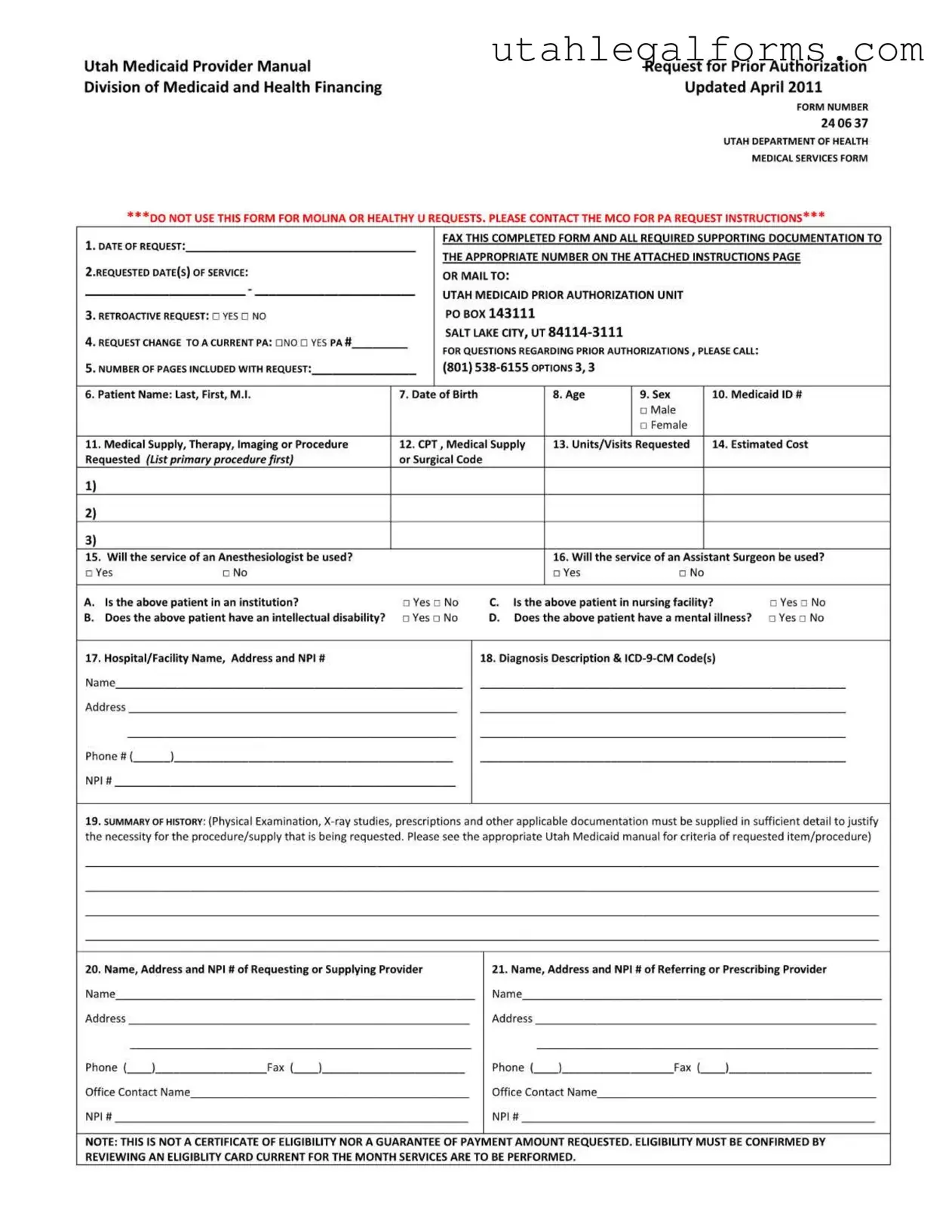
Fill a Valid Utah 24 06 37 Template
Dos and Don'ts
When filling out the Utah 24 06 37 form, it is essential to follow specific guidelines to ensure the request is processed efficiently. Below is a list of things to do and avoid:
- Do complete all required fields accurately and legibly.
- Do check the appropriate boxes for retroactive requests and changes to current prior authorizations.
- Do include all necessary supporting documentation to justify the request.
- Do ensure that the Medicaid ID number is entered correctly, as it is critical for processing.
- Do fax or mail the completed form to the correct address as specified in the instructions.
- Don't submit the form for Molina or Healthy U requests, as these require different procedures.
- Don't leave any mandatory fields blank; incomplete forms may be returned.
- Don't include codes from previous pages unless specified for additional entries.
- Don't forget to provide a summary of the patient's history; this is necessary for justification.
- Don't send the form without confirming the eligibility card is current for the service month.
More PDF Forms
Utah State Tax Form for Employees - The form covers a range of fuel types, reflecting diverse industry needs.
Tc 738 Utah - If represented, all official correspondence regarding the appeal will be directed to the designated representative.
The Arizona Motor Vehicle Bill of Sale form is a crucial document that records the transfer of ownership for a vehicle in Arizona. This form provides essential details about the buyer, seller, and the vehicle itself, ensuring a smooth transaction. Understanding how to properly fill out and use this form, which can be accessed through arizonapdfforms.com/motor-vehicle-bill-of-sale, can help prevent future disputes and streamline the registration process.
Utah State Tax Form - Utah State Tax Commission requires this form if specific boxes are checked on the return.
Listed Questions and Answers
-
What is the Utah 24 06 37 form?
The Utah 24 06 37 form is a request for prior authorization used by healthcare providers to obtain approval for specific medical services, therapies, or supplies under Utah Medicaid. This form must be completed accurately and submitted to the appropriate Medicaid authority.
-
Who should use this form?
This form is intended for healthcare providers seeking prior authorization for services covered by Utah Medicaid. It should not be used for requests related to Molina or Healthy U. Providers should contact the respective managed care organization for those requests.
-
What information is required on the form?
Key information includes:
- Date of request
- Patient’s name, date of birth, and Medicaid ID number
- Requested dates of service
- Details of the medical supply, therapy, or procedure
- Diagnosis description and relevant codes
All sections must be completed legibly to avoid delays.
-
Can I request retroactive authorization?
Yes, you can request retroactive authorization by checking the "YES" box on the form. This applies if the service date is prior to the request date. Ensure you provide all necessary details to justify the retroactive request.
-
How should I submit the completed form?
You can submit the completed form via fax or mail. If faxing, use the specific numbers provided for different types of requests. If faxing is not available, mail the original form to the Medicaid Prior Authorization Unit at the address listed in the instructions.
-
What happens if I do not provide all required information?
If any required information is missing or incorrect, the request will be returned without being processed. It is essential to double-check all entries before submission.
-
Is there a contact number for questions about the form?
Yes, for questions regarding prior authorizations, you can call (801) 538-6155 and select options 3, 3 for assistance.
-
What should I include with the request?
Along with the completed form, include any supporting documentation that justifies the necessity of the requested service. This may include medical history, examination results, and relevant prescriptions.
-
What is not covered by this form?
This form is not a guarantee of payment or eligibility. It is simply a request for authorization. Eligibility must be confirmed through the Medicaid eligibility card for the month in which services are to be performed.
-
What if I need to change a current prior authorization?
If you need to request a change to an existing prior authorization, indicate this on the form and provide the current prior authorization number. This will help streamline the process for your request.
Key takeaways
- Form Usage: Use the Utah 24 06 37 form exclusively for requests related to Utah Medicaid. Do not use it for Molina or Healthy U requests.
- Submission Method: Fax the completed form and all required documents to the appropriate number listed in the instructions. If faxing is not an option, mail the original form to the specified address.
- Completeness: Ensure all bolded sections are filled out clearly and accurately. Incomplete forms will be returned without processing.
- Patient Information: Provide the patient's full name, date of birth, age, sex, and Medicaid ID number. This information is crucial for processing.
- Service Details: List the medical supply, therapy, imaging, or procedure requested. Include up to three entries on the first page; additional requests can be made on page two.
- Cost Estimates: Include the estimated cost for each requested service. This helps in budgeting and planning for the procedure.
- Diagnosis Codes: Provide a detailed diagnosis description along with the corresponding ICD-9-CM codes to justify the request.
- History Summary: Include a narrative summary of the patient’s medical history. This should detail any relevant examinations, studies, or prescriptions.
- Contact Information: Clearly list the names, addresses, and NPI numbers for both the requesting and referring providers to facilitate communication.
Documents used along the form
The Utah 24 06 37 form is essential for requesting prior authorization for medical services under Medicaid. Several other documents often accompany this form to ensure that all necessary information is provided for a complete review. Below is a list of common forms and documents that may be used alongside the Utah 24 06 37 form.
- Medicaid Eligibility Verification Form: This document confirms the patient's eligibility for Medicaid benefits. It provides essential information about the patient's Medicaid status at the time of service.
- Physician's Order: A written order from the healthcare provider detailing the requested services or supplies. This order must be signed and dated by the physician to validate the request.
- Clinical Documentation: Includes medical records that support the necessity of the requested services. This may consist of history and physical examinations, lab results, or imaging studies.
- ICD-10 Diagnosis Codes: A list of diagnosis codes that provide a detailed explanation of the patient's condition. These codes are necessary for proper billing and justification of services.
- CPT Procedure Codes: Current Procedural Terminology codes that describe the medical procedures or services being requested. Accurate coding is critical for reimbursement.
- Prior Authorization Cover Letter: A cover letter summarizing the request and outlining the medical necessity for the services. This letter can help clarify the request for the reviewer.
- Patient Consent Form: A signed document from the patient authorizing the release of their medical information to the Medicaid provider. This ensures compliance with privacy regulations.
- Billing Information Sheet: A sheet that details the expected costs associated with the requested services. This helps in assessing the financial aspects of the request.
- Additional Documentation for Special Requests: Any extra forms or documentation required for specific services, such as durable medical equipment or specialty therapies, which may have unique requirements.
- Boat Bill of Sale: To ensure a seamless transfer of ownership when buying or selling a boat, it is crucial to utilize the appropriate documentation such as the legalpdf.org, which provides a comprehensive California Boat Bill of Sale form.
- Follow-up Request Form: Used to request changes or updates to an existing prior authorization. This form ensures that all modifications are documented and processed appropriately.
These documents collectively support the prior authorization request process, ensuring that the necessary information is available for a thorough review. Properly completed forms and accompanying documentation can significantly enhance the chances of approval for requested services.
File Specifications
| Fact Name | Description |
|---|---|
| Form Purpose | The Utah 24 06 37 form is used to request prior authorization for medical services under Utah Medicaid. |
| Governing Laws | This form is governed by the Utah Medicaid Provider Manual and the Division of Medicaid and Health Financing regulations. |
| Update Date | The form was last updated in April 2011, indicating the need for users to check for any changes or updates. |
| Usage Restrictions | It is important to note that this form should not be used for Molina or Healthy U requests; separate instructions apply. |
| Patient Information | The form requires detailed patient information, including name, date of birth, Medicaid ID, and sex. |
| Service Details | Requestors must list the medical supply, therapy, imaging, or procedure requested, with up to three entries allowed on the first page. |
| Documentation Requirements | Supporting documentation must be included to justify the necessity of the requested service, as outlined in the Medicaid manual. |
| Submission Instructions | Completed forms can be faxed or mailed to the appropriate Medicaid Prior Authorization Unit, with specific numbers for different types of services. |
| Eligibility Confirmation | The form is not a guarantee of payment; eligibility must be confirmed through the Medicaid eligibility card valid for the service month. |
| Contact Information | For questions regarding prior authorizations, users can call the Medicaid office at (801) 538-6155. |